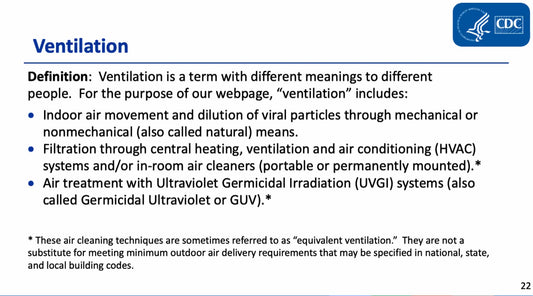
In healthcare facilities, the effectiveness of ventilation and air quality management is paramount in safeguarding patients and healthcare workers. These systems play a crucial role in reducing the risk of disease transmission, ensuring a safe and comfortable environment, and improving overall infection prevention strategies. Standard 241 by ASHRAE can now be adhered to reduce infectious aerosols in our indoor environments.
Airborne transmission is a concerning method of pathogen spread within healthcare settings. Pathogens hitch a ride on dust particles or aerosolized respiratory droplets, traveling substantial distances on air currents. Notable examples of illnesses typically transmitted this way include measles, varicella-zoster, and tuberculosis. Other respiratory diseases like COVID-19, pertussis, and influenza can also spread through respiratory droplets but often over shorter distances.
To mitigate these risks, healthcare facilities employ various levels of control measures. The first line of defense is hazard elimination. Following that, engineering controls come into play, influencing the built environment. HVAC systems, as part of these engineering controls, are instrumental in reducing the transmission of airborne pathogens and minimizing exposure risk.
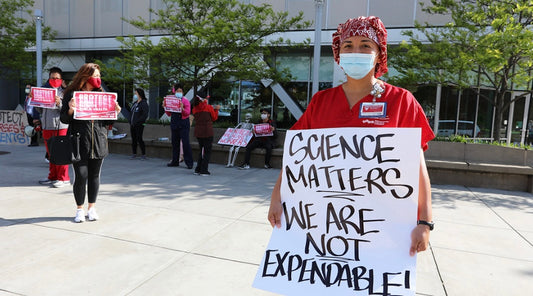
Several studies have underscored the pivotal role of ventilation, especially during the COVID-19 pandemic. Increased ventilation and the strategic direction of airflow away from at-risk individuals have been shown to decrease the risk of infection in numerous instances.
Regulatory and professional organizations have published comprehensive guidelines for the functioning of HVAC systems within healthcare facilities. Infection preventionists (IPs) must have a firm grasp of these guidelines, including those set forth by the Facility Guidelines Institute (FGI), American Institute of Architects, and the American Society of Heating, Refrigerating, and Air-Conditioning Engineers, in line with local and state health department requirements.
Key principles IPs need to comprehend in terms of ventilation and disease prevention encompass quantity (measured by air changes per hour [ACH]), quality (evaluating air filtration and contamination levels, temperature, and humidity), and flow (focusing on pressure differentials influenced by the volume of air supplied versus removed and its direction).
Quantity, in particular, plays a vital role in disease transmission control by effectively eliminating contaminated air from enclosed spaces. As air changes increase, particle removal efficiency rises. For critical areas like operating rooms, a higher minimum ACH is required compared to less critical patient care zones. The implementation of other mitigation strategies, such as masks and respirators, is essential for close-range contact.
Air quality can be influenced by both outdoor and indoor factors. Outside air infiltrates through leaks, windows, doors, and HVAC system filtration issues. Construction near critical areas or intake vents can introduce contaminants if not correctly filtered. Monitoring outside air quality is essential, especially during events like wildfires, industrial accidents, or high pollution levels. Maximizing the use of outdoor air for HVAC intake is generally recommended, particularly in comparison to mixed air that includes recirculated air.
The humidity levels within healthcare facilities can also impact disease transmission. Lower humidity can extend the distance aerosolized particles can travel and their suspension time.
Filtration is another integral component of HVAC systems, designed to improve air quality by capturing particles. High-efficiency particulate air (HEPA) filters are commonly used in healthcare settings. These filters are efficient at trapping smaller particles and are recommended in areas where enhanced filtration capabilities provide a clinical advantage.
Additionally, during the COVID-19 pandemic, portable HEPA filters and negative pressure machines have been valuable in complementing existing HVAC systems.
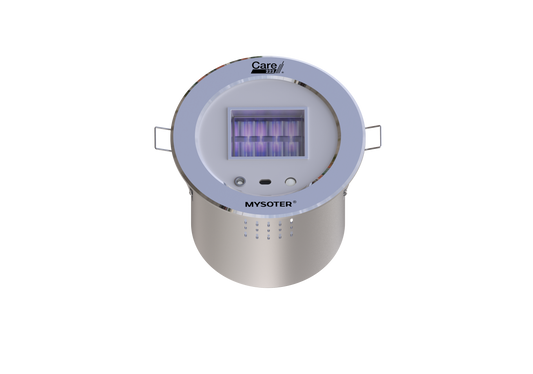
Innovations in air disinfection have also emerged, with UV radiation, particularly Far UV-C at 222nm, being effective at pathogen inactivation. While being safe for human skin and eyes we can safely disinfect areas continuously. Far UVC in addition to great air purification can be a great way to improve ventilation in healthcare settings.
To enhance the understanding of HVAC systems and their role in disease prevention, IPs should collaborate with facilities and engineering teams. By using Far UVC in areas where air flow is poor like dining areas or high traffic places it can strongly reduce any airborne or surface pathogens. IPs bring clinical and disease transmission expertise to the table, while the facilities and engineering teams provide invaluable insights into the built environment.
Infection Risk Management Mode, which is stated heavily in ASHRAE's Standard 241, also necessitates the incorporation of air quality considerations. Remodeling or new construction projects offer opportunities to enhance HVAC systems with features like Far UVC disinfection, improved filtration, and increased outdoor air usage. These engineering controls, coupled with robust IP foundations, form a multifaceted approach to reduce the risks of airborne pathogen transmission, ensuring safer and more resilient healthcare facilities.